Recovery After Prosthesis Surgery: A Comprehensive Guide
The hip and knee joints are joints that are actively used in everyday life. Due to arthritis or trauma, these joints may not be used as actively as before. In this case, joint replacement surgery may be necessary to restore the joints to their former function. These surgeries are performed to improve patients’ quality of life and reduce their pain. Patients can then return to their daily lives, work or favorite activities.
Joint replacement surgery is a permanent treatment. However, patients also have a number of responsibilities for a successful outcome. The healing process starts with preoperative preparations. After surgery, patients should learn what to expect and take precautions accordingly. It is important to remember that recovery is a time demanding process and that there are different needs at each stage.
Expectations from Joint Replacement Surgery
Setting clear expectations is important for a successful recovery after joint replacement surgery. When you understand what to expect after hip replacement surgery or knee replacement, you are more likely to be satisfied with the outcome and adapt to your new lifestyle with confidence.
Your individual condition plays a major role in the results of the surgery. Several factors may influence your recovery, including:
- Pre-surgery Pain and Mobility: Severe pain or limited function before surgery may slow your recovery.
- Existing Health Conditions: Obesity, diabetes, hypertension, or heart disease can affect healing and long-term outcomes.
- Lifestyle Habits: Smoking, for example, impairs blood flow and may delay recovery.
These factors don’t rule out success, but they highlight why outcomes differ between patients. Discussing your situation with your surgeon ensures a clearer picture of what to expect.
A successful hip or knee replacement recovery starts with open communication. During pre-surgery consultations:
- Review your medical history in detail, including chronic conditions and medications.
- Discuss achievable milestones, such as pain reduction, improved mobility, and return to daily activities.
- Address lifestyle adjustments—like weight management or quitting smoking—to improve results.
Unrealistic goals—such as expecting zero hip or knee pain after replacement or complete restoration of youthful function—can lead to frustration. Instead, focus on measurable progress: walking with less discomfort, climbing stairs more easily, or resuming hobbies. By understanding the likely timeline and limitations, you’ll feel more empowered and satisfied with your progress.
Your surgeon is your partner in setting achievable targets. Ask questions, voice concerns, and clarify doubts before surgery. A well-informed patient is better prepared to adapt to post-surgery life.
First 24 Hours After Joint Replacement Surgery

The first 24 hours after joint replacement surgery are important for your knee or hip replacement recovery. During this time, your medical team will closely monitor your condition, manage pain, and help you take the first steps toward rehabilitation.
Monitoring Vital Signs
After surgery, your medical team will focus on stabilizing your condition. This includes:
- Tracking Vital Signs: Heart rate, blood pressure, and oxygen levels are monitored to ensure your body is recovering well.
- Managing Side Effects: If you experience nausea, vomiting, or dizziness from anesthesia, medications will be provided to ease these symptoms.
- Medications: You’ll receive pain medication after knee replacement or hip replacement surgery to manage discomfort. Blood thinners may also be administered to prevent blood clots, and antibiotics to reduce the risk of infection.
Physiotherapist Guided First Movement
A few hours after surgery, your physiotherapist will help you get out of bed and take your first steps.
- Rehabilitation Starts Early: While some patients may walk the same day, others with conditions like low blood pressure may need to wait until the next day.
- Walking After Knee Replacement or Hip Replacement: With the assistance of a walker or crutches, you’ll begin walking short distances. This improves blood circulation, reduces swelling, and lowers the risk of complications like deep vein thrombosis (DVT).
Customized Rehabilitation Plan
Your recovery plan is tailored to your needs. In the hospital and later at home, your physiotherapist will explain:
- How to safely get in and out of bed, sit and stand.
- How to use orthopedic devices.
- Tips for walking after knee or hip replacement.
- The correct way to climb stairs after knee replacement.
- Recommended exercises after hip replacement or knee replacement to improve strength and flexibility. These exercises should be started within 24 hours after surgery.
- Proper lying, sitting, and bending positions to protect the operated joint.
Your caregiver or accompanying person should also pay attention to these instructions, as they’ll play an important role in supporting you at home.
Use of CPM (Continuous Passive Motion) Machine
Your doctor may recommend using a CPM machine for knee replacement or hip replacement. This device gently moves your joint to:
- Reduce pain and swelling.
- Improve range of motion and joint flexibility.
- Speed up recovery and prepare you for discharge.
The CPM machine is typically used for up to 8 hours a day, excluding sleep and physical therapy. It may be started within 24 hours after surgery and may be continued at home for about 2 weeks.

Use of DVT (Deep Vein Thrombosis) Treatment Device
As with many operations, there is a risk of DVT after hip replacement or knee replacement. Deep vein thrombosis (DVT) is a blood clot that forms in veins deep inside the body. The veins in the legs have small valves that help the blood to move towards the heart. DVT can damage these valves.
In most cases, clot appears in one of the veins in the lower leg. In more serious stages, it can reach the lung and cause pulmonary embolism (lung clot). To reduce this risk, your medical team may use a DVT treatment device.
The DVT treatment device consists of cuffs that wrap around your legs. These cuffs inflate with air and apply gentle pressure to improve blood flow and prevent clots. The device increases blood flow and reduce the risk of DVT.
The device is typically started immediately after surgery and used continuously for about 1 week. By following your doctor’s recommendations for DVT prevention, you can significantly lower your risk of complications.

Hospital Discharge Process
The discharge after knee replacement or hip replacement process is a significant step, but it’s important to leave the hospital only when you’re medically ready. The timing of your discharge depends on how quickly you recover, but most patients stay in the hospital for 1 to 4 days. However, being discharged too early without meeting certain criteria can negatively affect your recovery. To ensure a safe and smooth transition from the hospital to home, there are specific goals you need to achieve before leaving.
Before you are discharged after knee replacement or hip replacement, your medical team will check if you meet the following requirements:
- Move Independently: Safely get in and out of bed without assistance.
- Managing Pain Effectively: Your pain should be reduced to an acceptable level.
- Eat and Drink Normally: You should be able to consume food and fluids without difficulty.
- Using the Toilet Safely: After prosthesis surgery, you should be able to use the bathroom without difficulty.
- Walking Short Distances: With the help of an orthopedic device like a walker, cane, or crutches, you should be able to walk a short distance.
- Climbing Stairs: You should be able to climb up and down two to three steps of stairs after knee replacement or hip replacement.
- Perform Home Exercises: You should be familiar with the exercises recommended for your recovery.
- Understanding Safety Precautions: It’s important to know how to prevent accidents, such as falls, during your recovery.
If you’re unable to meet these goals, your stay may be extended to ensure you receive the necessary care.

First 2 Weeks at Home After Joint Replacement Surgery
The first two weeks at home after knee or hip joint replacement surgery are an important period in your recovery. During this time, careful attention to your wound care, personal hygiene, exercise, and safety can make a significant difference. It is important to follow your doctor’s instructions closely to avoid infection, blood clots, and other complications.
Wound Care and Stitches
After hip or knee replacement surgery stitches, your surgical wound requires careful attention to prevent infection. On average, your stitches will be removed around 14 days after surgery, though this timeline may vary depending on your healing progress. Until then, it’s necessary to follow these steps for proper wound care after knee replacement or hip replacement:
- Do not allow any water or liquid to come into contact with your stitches or the wound area. Since you won’t be able to shower during this time, take sponge baths to keep your body and the area around the wound clean.
- After the first dressing is removed, you can shower with a waterproof dressing.
- Dressing and bandaging of the surgical wound are first applied in the operating room. On average, the dressing for knee replacement or hip replacement needs to be renewed and the bandage changed every 3-4 days.
- In some cases, such as discharge, it may be necessary to apply dressings and change the bandage every day. For this procedure, you can go to a full range of health centers. It can also be done at home if the necessary hygienic conditions are met.
- Surgical stitches are removed in the clinic. In some cases, the stitches do not need to be removed because they are placed under the skin.
- Do not immerse the wound in water until 6 weeks after surgery. Therefore, do not enter the water in environments such as bathtubs, pools and the sea.
- After your stitches are removed, you can take a bath or shower and start walking without an assistive walking aid.
After hip or knee replacement wound leaking, redness, swelling, or warmth are signs of infection. If you notice any of these, contact your doctor immediately. Proper care of your stitches is important to prevent complications that could delay your recovery.

Common Symptoms After Surgery Joint Replacement Surgery
After knee joint replacement or hip joint replacement surgery, experiencing certain symptoms is a normal part of the healing process. While some symptoms may feel unsettling, many are normal and part of the healing process. Understanding what is normal can help you feel more at ease during your recovery. Managing these symptoms can improve your overall recovery.
- Pain: Mild to moderate discomfort is typical, especially in the first few weeks. Then, what is normal pain after hip replacement surgery or knee replacement? Aching around the incision site or during movement is common and should gradually improve.
- Swelling: Swelling after knee replacement or hip replacement is usually noticeable for 2 to 3 weeks. In some cases, it may continue for 3 to 6 months.
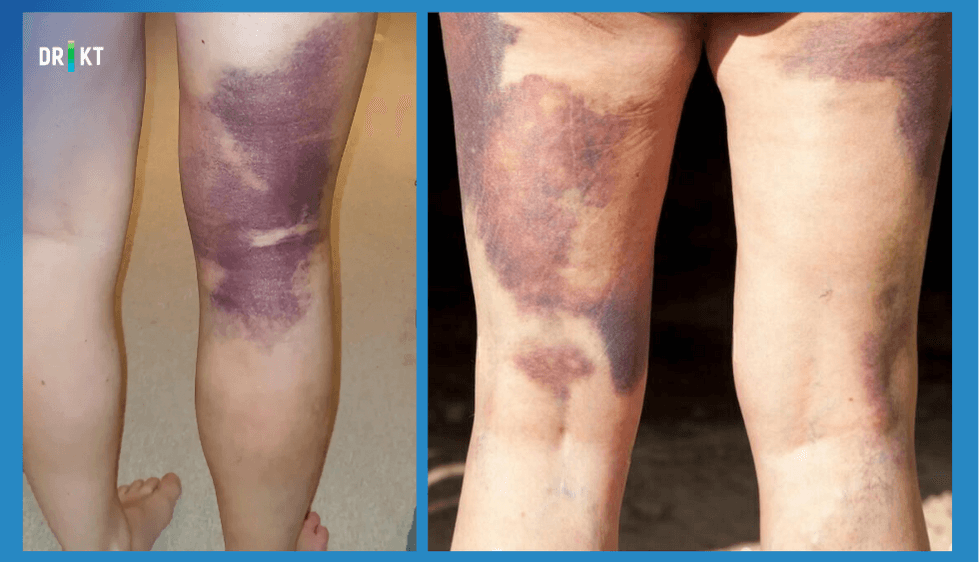
- Bruising: Bruising after knee replacement or hip replacement can last between 1 and 2 weeks. This is a normal response to surgery and should gradually fade.
- Clicking Noises: A clicking noise after knee replacement or hip replacement is often heard and is generally not a cause for concern. This sound occurs as the new joint components adjust to your movements. Over time, the noise should decrease. However, if the clicking is accompanied by pain, swelling, or any deformity in the joint, consult your doctor to ensure everything is functioning properly.
Managing Pain After Joint Replacement Surgery
While knee and hip replacement surgeries aim to relieve chronic pain, it’s normal to experience temporary discomfort during recovery. Understanding how to manage pain after knee replacement or pain in replaced hip joint can help you stay comfortable and support healing.
This pain is usually most intense in the first few days and gradually improves. However, unmanaged pain can slow recovery, thus it’s important to address it effectively. Your doctor will recommend a personalized plan, but the following strategies are often effective:
- Medication: Use prescribed painkillers as directed. Opioids may be used for severe pain initially, but non-opioid options are preferred for long-term use to avoid side effects.
- Cold Application: Applying an ice pack for knee replacement or hip surgery areas can reduce swelling, numb pain, and ease inflammation.
- Physical Activity: Staying moderately active can prevent muscle stiffness and cramps. Avoid remaining in the same position for too long, as this may worsen pain.
- Rest: Balance activity with adequate rest. Overexertion can lead to increased pain, so follow your doctor’s guidelines on how much rest is needed.
- Changing Positions While Resting: If you spend a lot of time lying down, change your position every 2 hours to prevent muscle strain and back pain. Proper alignment of your hips, back, and head can also reduce unnecessary pressure on your joints.
- Aromatherapy: Some patients find relief through essential oils after knee replacement surgery or hip replacement. Aromatherapy uses natural scents like lavender or eucalyptus to promote relaxation and reduce pain, anxiety, and insomnia.
- Massage Therapy: Once your stitches are removed, massage after knee replacement or hip replacement can relieve muscle tension and improve blood flow. Techniques like effleurage (gentle stroking) are effective.
- Shower: You should not expose the wound to any liquid until your stitches are removed. However, taking a warm shower after your stitches are removed can reduce your pain, relax your muscles and help you relax.
- Breathing Techniques: Deep breathing exercises can lower stress, reduce pain, and improve oxygen flow to healing tissues.
- Comfort Adjustments: Create a restful environment by dimming lights, adjusting room temperature, and reducing noise.

Managing Swelling After Joint Replacement Surgery
Swelling around the surgical area is a common and expected part of recovery after a joint replacement procedure. While swelling usually decreases gradually over a period of up to six months, managing it effectively can speed up healing and improve comfort. To reduce swelling after hip replacement or knee replacement, consider these methods:
- Leg Elevation: Keep the operated leg raised above heart level when sitting or lying down. Use pillows for support. This helps drain excess fluid and reduces swelling after hip replacement or knee surgery.
- Ice Application: Use cold packs or ice wrapped in a cloth on the swollen area for 15–20 minutes, several times a day. Avoid placing ice directly on the skin to prevent frostbite.
- Exercise: Gentle movements recommended by your physiotherapist improve circulation and reduce fluid retention. Avoid overexertion, which can worsen swelling.
If you notice a sudden or severe increase in swelling during your recovery, contact your doctor immediately, as this may indicate an infection.
Managing Bruising After Joint Replacement Surgery
Bruising around the surgical site is a common and temporary side effect of hip replacement or knee replacement procedures. Bruising develops when small blood vessels under the skin are damaged during surgery, causing blood to pool. While it may look concerning, mild to moderate bruising after hip replacement or knee surgery typically fades within 1–2 weeks.
Your doctor may prescribe blood thinners to reduce the risk of deep vein thrombosis. These medications can sometimes increase the appearance of bruising. To manage and reduce bruising, you can follow these steps:
- Elevate the Affected Leg: Keep your leg raised above heart level when resting. This minimizes blood pooling and reduces swelling and bruising.
- Avoid Strain on the Area: Refrain from sudden movements or massaging the bruised skin, which can worsen discoloration.
- Cold Compress: Applying an ice pack or cold compress to the affected area can limit swelling and discoloration.
You should contact your doctor if the bruising spreads significantly or becomes more intense over time.
Potential Complications After Joint Replacement Surgery
Joint replacement procedures are generally safe, but like any surgery, they can have complications. These complications depend on factors such as your overall health, age, and how closely you follow your doctor’s instructions. Below are some issues that can occur after a joint replacement procedure, along with ways to manage them.
Blood Clot or Deep Vein Thrombosis (DVT)
One of the most significant risks after joint surgery is developing a blood clot after knee replacement or hip replacement, also known as deep vein thrombosis (DVT). DVT occurs when a clot forms in a deep vein, often in the legs. If left untreated, it can travel to the lungs (pulmonary embolism) or brain.
Signs of blood clot after knee replacement or hip replacement surgery may include:
- Swelling in one leg.
- Redness or warmth around the affected area.
- Pain or tenderness, especially when standing.
To reduce the risk of DVT after knee replacement surgery or hip replacement, your doctor might recommend:
- DVT Treatment Devices: These help improve blood flow in the legs.
- Lower Leg Exercises: Regular movement can prevent blood stagnation.
- Leg Elevation: Keeping your legs elevated improves circulation.
- Blood Thinners: These medications reduce the likelihood of clot formation.
Infection Risks
Though rare, an infection in knee replacement or hip implants is a serious complication requiring immediate treatment. Bacteria can enter the surgical site during or after the procedure, leading to localized or systemic infection. Watch for signs such as:
- Increased redness, warmth, or swelling at the incision.
- Persistent or worsening pain.
- Unusual odor or discharge from the wound.
- Stitches opening or separating.
- Fever or a general feeling of illness.

To prevent infection after a joint replacement procedure:
- Maintaining Hygiene: Pay close attention to wound care, especially during the first two weeks before your stitches are removed. Keep the area clean and dry to prevent contamination.
- Pre-surgery Preparation: Stop smoking at least four weeks before surgery and avoid alcohol two weeks prior to the procedure, as these habits can impair healing.
- Antibiotics: Take all prescribed antibiotics as directed, both before and after surgery, to protect against bacterial infections.
- General Health Measures: Strengthen your immune system by eating a balanced diet, staying hydrated, and getting adequate rest.
Managing Postoperative Medications
After joint replacement surgery, your doctor will prescribe medications tailored to your needs. They help reduce pain, manage side effects, prevent blood clots, and ward off infection. In many cases, these medications work together with physiotherapy to help you return to your normal activities.
Pain Control
Managing pain is an important part of your recovery. If you experience intense pain, starting rehabilitation can be difficult. Using the painkillers your doctor has prescribed can help you move more easily and begin physical therapy sooner.
Managing Medication Side Effects
Post-surgery drugs, including opioids or blood thinners, can sometimes cause side effects such as nausea, vomiting, or constipation. Studies shows that up to 55% of patients experience these issues. With your doctor’s guidance, you can use anti-nausea or stool softeners to ease these symptoms. You should not take any medicine that your doctor has not prescribed or approved.
Blood Thinners
After a joint replacement procedure, there is a risk of blood clots. These clots can develop in deeper veins, a condition known as deep vein thrombosis (DVT). If a clot breaks loose, it can travel to critical areas of the body. To lower the risk of blood clots, your doctor might recommend:
- Blood Thinners: Medications that help prevent clot formation.
- Compression Devices: Tools that improve blood circulation in your legs.
- Leg Elevation and Exercises: Simple movements that boost circulation.
Preventing Infections
Infections are another potential complication after joint replacement surgery. While your immune system typically fights off harmful bacteria, certain factors can increase your risk of infection:
- Conditions like diabetes, obesity, circulatory problems, or weakened immunity (e.g., HIV) can make you more vulnerable.
- Infections can occur at the surgical site or spread to the prosthetic joint area.
To reduce this risk, your doctor will prescribe antibiotic medications before and after surgery. Additional precautions include:
- Maintaining good personal hygiene.
- Caring for the surgical site carefully.
If you notice any signs of infection, such as redness, swelling, or discharge, contact your doctor immediately.
Physical Therapy and Exercise After Joint Replacement Surgery
Starting a physical therapy and exercise program after joint replacement surgery is important to manage your recovery effectively. Customized exercises help build strength, improve joint movement, and increase flexibility in your knee or hip.
The rehabilitation process begins as soon as you wake up after surgery. In the hospital, you will start with gentle movements that continue at home. Studies show that joint replacement physical therapy initiated within the first 24 hours can help control pain and speed up early recovery.
After surgery, you may experience stiffness or discomfort that makes movement challenging. Taking the pain medication recommended by your doctor can help you participate fully in your therapy. Focusing on the long-term benefits of exercise can also keep you motivated throughout your recovery.

The advantages of an exercise regimen and structured physical therapy after knee replacement or hip replacement include:
- Pain Relief: Regular exercise helps reduce postoperative pain over time.
- Reduced Inflammation: Movement improves circulation, which decreases swelling and inflammation.
- Improved Circulation: Exercise promotes healthy blood flow, reducing the risk of complications like blood clots.
- Regained Joint Strength and Mobility: Targeted routines rebuild strength and range of motion.
- Stronger Surrounding Muscles: The muscles around your knee or hip joint will stabilize and support your new prosthesis.
- Decreased Joint and Muscle Stiffness: Physical therapy helps loosen stiff joints and muscles, making movement easier.
- Better Balance and Coordination: Exercises improve your stability, reducing the risk of falls.
- Improved Gait: You’ll walk more naturally as your joint regains function.
- Faster Recovery: A consistent program helps you resume daily tasks.
It is normal to feel some soreness or mild swelling after exercise. Do not stop your routine because these symptoms are a part of the healing process. If needed, manage discomfort with your prescribed medication or by applying ice. However, if the exercises after hip replacement or knee replacement become too challenging, stop the activity and consult your doctor.
Adapting to Daily Life After Joint Replacement Surgery
Returning to everyday activities after joint replacement surgery requires patience, care, and attention to detail. Knowing what to expect and how to safely navigate everyday activities can make your transition smoother and more comfortable.
Movements to Avoid After Surgery
It is important to be cautious with your movements. For patients who have undergone hip or knee replacement surgery, note the following:
After Knee Replacement Surgery:
- Avoid activities that may twist or overstrain your knee in the early stages of recovery.
- Don’t force bending or straightening your knee if it causes pain. Gradually increase your range of motion as guided by your therapist.
- Take small, controlled steps when turning, and avoid turning on your operated leg.
- Refrain from sudden movements with your knee.
After Hip Replacement Surgery:
- Be aware of hip replacement activities to avoid, such as crossing your legs for 6–8 weeks, lifting your knee higher than your hip, or leaning forward when sitting.
- Avoid bending your lower back more than 90 degrees.
- Be cautious about bending over to pick something up or pulling blankets while lying in bed.
- Do not turn your feet inward or outward excessively when bending over.
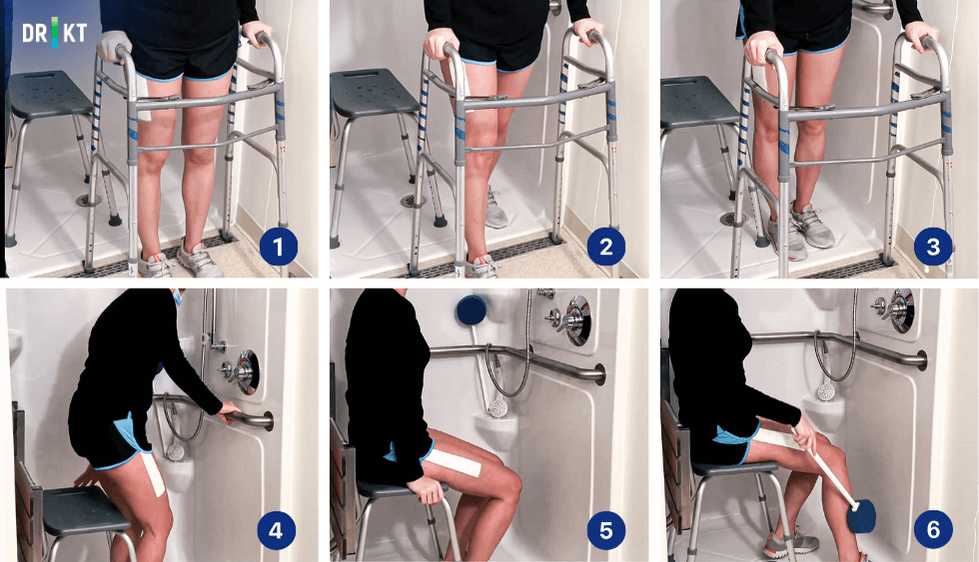
Showering After Surgery
Bathing or showering after hip replacement and knee surgery requires extra care to prevent falls and protect the incision. It is important to make appropriate preparations before surgery and to organize your bathroom for the postoperative period. The bathroom should be made safe as it is an area where there is a high risk of falls.
Until your stitches are removed (usually around 2 weeks), avoid exposing the wound to water. Until then, sponge baths are recommended to keep the surgical site dry and safe.
Getting in and out of bath after hip replacement or knee replacement may differ depending on the bathroom layout in your home. If you have a bathtub at home, you can take a bath by following the instructions below:

- To make it easier to get in and out of the bathtub, you should first get a bathtub transfer bench.
- Place the bathtub transfer bench in a suitable position.
- Sit on the tub transfer bench with your back to the tub.
- Turn into the tub and take turns lifting your legs up and in.
- Follow the same steps in reverse when getting out of the bathtub.
If you have a shower cabin in your home, you can take a shower by following the steps below:
- It is recommended to get a bath chair first.
- When getting in and out of the shower, move by stepping sideways.
- Sit on the bath chair during the shower.
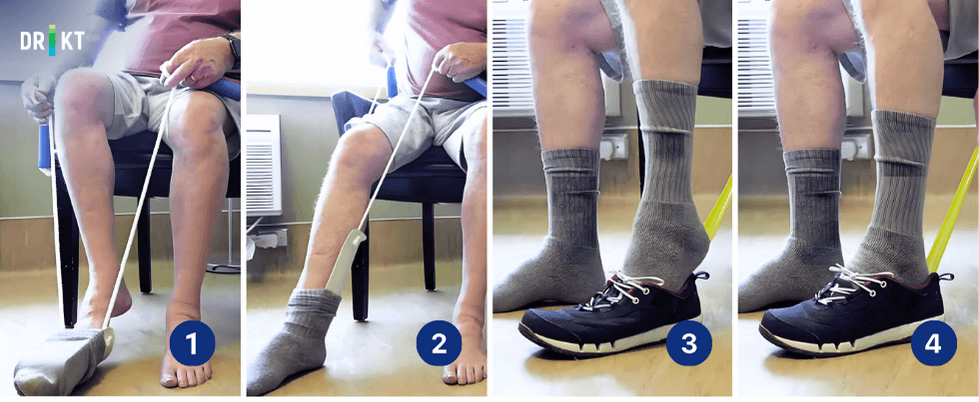
Getting Dressed Safely
When getting dressed after hip replacement or knee replacement, follow these steps to avoid strain:
- Sit on a chair or the edge of your bed while dressing to maintain balance and avoid falls.
- Use dressing aids like a shoehorn to avoid bending.
- When putting on clothes, start with the operated side first (e.g., pants or socks). When removing clothes, start with the non-operated side.
Sleeping Positions
Understanding how to sleep after knee replacement or hip replacement is important for proper sleep.
Recommendations for lying position after hip replacement surgery are as follows:
- Sleeping on your back is the safest option. Avoid sleeping on your stomach or the operated side.
- Place a pillow between your knees to keep them aligned and prevent inward rotation.
- Avoid bending your knees excessively or placing pillows under your knees.
- You can change position if you feel uncomfortable.
The safest sleeping position recommendations after knee replacement surgery are as follows:
- Lying on your back is ideal, as it keeps your legs straight and promotes healthy blood flow.
- You can place a pillow under your calf for support, but avoid bending your knee too much.
- Wait several weeks before sleeping on your side, and avoid lying directly on the operated area.

Returning to Work
How long off work for knee replacement or hip replacement depends on how much physical activity your job involves and how your recovery progresses. Thus, it can take anywhere from a few days to several weeks to return to work. You should consult your doctor to decide when it is safe to resume your professional activities.
Returning to Sports and Physical Activities
You should follow the exercise program created by your physiotherapist for at least 2 months. In some cases, an exercise bike is also recommended to increase your knee/hip flexibility and strengthen your muscles. 3-6 months after your surgery, you can be more active in daily activities. You can return to sports that do not put too much strain on your knees or hips.
Another important issue to be aware of when returning to sport after knee replacement surgery or hip replacement is the risk of falling. If you have an accident or fall during sports, your recovery can be negatively affected. Therefore, you should avoid sports involving close contact and take measures to eliminate the risk of falling.
You should pay attention to the following points about returning to your active life:
- You can walk as far as you want. However, walking is not a substitute for the exercises recommended by your physiotherapist.
- One of the best physical activities after joint replacement surgery is swimming. Once your surgical wound has healed, you can start swimming again.
- It is recommended to do low-impact exercises such as golf, cycling and doubles tennis instead of sports that involve jumping, running and fast changes of direction, such as basketball, skiing and singles tennis.
Consult your doctor to determine which sports are suitable for you based on your progress.
Driving After Surgery
Driving requires strength, coordination, and quick reflexes, so it’s important to wait until you’re fully ready. When you are not taking opioid pain medication and your strength and reflexes are better, it is safe to drive. Everyone develops safe conditions for driving at a different time.
On average, you can drive 4 to 6 weeks after knee replacement surgery. After hip replacement surgery, you can drive a car after a few weeks or a month. You should always consult your doctor to determine the most appropriate driving date after surgery.
The Role of Nutrition in Recovery After Joint Replacement Surgery
A balanced and healthy diet ensures that your body receives the vitamins, minerals, and nutrients it needs to repair tissues, reduce inflammation, and regain strength. While supplements can be helpful, natural foods are more effective at providing essential nutrients because they are better absorbed by the body.
Before starting any new eating plan, consult your doctor and dietitian. They can advise you on the best diet after knee replacement surgery or hip replacement based on your individual needs.

Staying Hydrated
Hydration is one of the most important aspects of post-surgery recovery. Anesthesia and medications used during and after surgery can cause dehydration, which may lead to complications such as constipation or fatigue. Drinking plenty of water helps flush medications out of your system and supports overall healing.
Maintaining Electrolyte Balance
Electrolytes are essential minerals like sodium, potassium, magnesium, and calcium that help regulate vital functions such as hydration, muscle contractions, and pH balance. Surgery and anesthesia can disrupt your body’s electrolyte levels, so it’s important to replenish them through your diet. To maintain electrolyte balance, you can consume foods rich in electrolytes include bananas (potassium), spinach (magnesium), dairy products (calcium), and nuts (phosphorus).
Chewing Gum
Surgery and medications can disrupt digestion, leading to constipation or nausea. To support your digestive system, chew sugar-free gum to stimulate gastrointestinal motility.
Alcohol Consumption After Surgery
While recovering from surgery, it’s best to avoid alcohol entirely. Drinking alcohol after hip replacement or knee replacement can dehydrate your body and interfere with medications prescribed for pain management or blood thinning. Even after stopping medication, you should only consume alcohol in moderation and with your doctor’s approval.
Iron-Rich Foods
Surgery often leads to some degree of blood loss, making iron-rich foods particularly beneficial for recovery. Iron supports red blood cell production and helps combat fatigue. Include foods to your diet such as red meat, spinach, kale, beans, and dried fruits in your diet.
Anti-Inflammatory Diet
It is very effective to pay attention to nutrition to prevent inflammation in the operated area. Focus on antioxidant-rich foods such as pomegranates, cherries, beets, berries, and dark leafy greens to prevent inflammation. Also, embrace a Mediterranean-style diet, which includes fish, olive oil, nuts, seeds, whole grains, and plenty of fruits and vegetables. Avoid processed sugars, as they can increase inflammation and hinder recovery.
Eating Before Taking Medications
Take solid food before your medication. Eating prior to taking medicine protects your stomach and helps reduce the chance of nausea.
Dental Care After Joint Replacement Surgery
If you require dental work after knee replacement or hip replacement, timing is important to minimize the risk of infection:
- Before Surgery: Complete any non-urgent dental work (e.g., cleanings, fillings) at least 6 weeks before your joint replacement surgery.
- After Surgery: Avoid dental treatments for 3 months post-surgery unless it’s an emergency. This reduces the risk of bacteria reaching the surgical site.
This precaution is necessary because dental procedures can allow bacteria to enter the bloodstream, potentially leading to an infection in the joint prosthesis.
If dental treatment is unavoidable during this period, consult your doctor. They may recommend taking antibiotics before the procedure to reduce the risk of infection.

Recovery Progress: Week 2 to Month 3
Between the second week and the third month after joint replacement surgery, you may gradually regain mobility and reduce your reliance on orthopedic supports. Typically, within 3 to 6 weeks, you may no longer need a cane or walker. However, if you still require one, holding it on the opposite side of your operated knee or hip can help improve balance and walking stability.
During this period, you may also resume light daily activities. If you are no longer taking pain medication, your doctor may approve you to start driving again. Always consult your healthcare provider before making changes to your routine.
Consistently following your physical therapy program will help you regain strength and mobility. By this stage, most swelling and inflammation should have subsided. Your physical therapy exercises will continue to focus on improving your range of motion and strengthening the muscles around your joint. Generally, physical therapy is completed around two months after surgery, but recovery varies for each individual.
Recovery Progress: Month 3 to Year 1
As your recovery continues, it is important to stay active by walking regularly and avoiding prolonged sitting. Keeping your body in motion will help reduce pain and prevent stiffness in the operated joint. During this period, you should notice further improvements in your mobility and comfort.
By the third month, you may be able to resume most of your normal activities. However, complete recovery can take up to 12 months. One year after surgery, most patients experience little to no pain. However, some individuals may still have occasional mild discomfort. Recovery speed varies from person to person, so follow your doctor’s recommendations for the best results.
Conclusion
A successful knee or hip replacement surgery depends on various factors, including the surgeon’s expertise, advanced technology, and the chosen surgical method. Yet, patient commitment plays an important role in achieving the best outcome. Following medical advice before and after surgery significantly reduces the risk of complications.
This guide has provided insights on wound care, physical therapy, medication, nutrition, and daily activities during the recovery period. If you have any further questions or need more information, feel free to reach out to us through our website or social media channels.